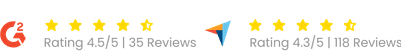
Trusted by Thousands of Happy Providers Since 2010!


Expert Medical Credentialing, Enrollment & Licensing Services
We help U.S. healthcare providers, specialists, and therapists get credentialed, enrolled, and compliant—without delays, confusion, or lost revenue
- Credentialing for providers & specialists
- Insurance enrollment for seamless reimbursements
- Hospital credentialing for smooth affiliations
- Ongoing credential maintenance to prevent coverage lapses
Our Stats
Trusted by
Commercial Insurance Credentialing
$200
per provider
- Credentialing application submission
- Insurance payer enrollment (Commercial plans)
- Real-time credentialing status tracking
- Follow-ups with insurance companies
- Application corrections & resubmissions
- Expert credentialing support
Medicare Credentialing
$250
per Provider
- Medicare enrollment (PECOS)
- Application submission & tracking
- Revalidation & updates
- Follow-ups with Medicare
- Appeals & resubmissions if required
- Dedicated credentialing assistance
Medicaid Credentialing
$250
per Provider
- State Medicaid enrollment
- Complete application handling
- Continuous follow-up with Medicaid offices
- Corrections, resubmissions & appeals
- Real-time status updates
- Professional credentialing support
Military / VA (TriWest) Credentialing
$250
per Provider
- TriWest / VA Community Care enrollment
- Provider credentialing & contracting support
- Application submission & document management
- CAQH verification & updates
- Continuous follow-ups with TriWest / VA
- Corrections, resubmissions & appeals (if required)
- Real-time status tracking
- Expert credentialing support
End-to-End Credentialing & Enrollment Services
We handle the complexities of medical credentialing, so you don’t have to.
Our experienced credentialing specialists manage the full process accurately and efficiently—ensuring you stay compliant and get paid on time.
- Medicaid & Medicare Enrollment
- Commercial Insurance Credentialing (Aetna, Humana, BCBS, UnitedHealthcare, etc.)
- Hospital Privileging & Managed Care Contracting
- NPI Registration (Type I & Type II)
- Re-Credentialing & Ongoing Compliance Support
- CAQH Registration & Maintenance
- Reimbursement Issue Resolution
Medical Credentialing Company
Trusted by 200+ Practices
See how healthcare providers rate our insurance credentialing services on Trustpilot.







Mosiah Wilson
Brawta Psychiatric ✅
★★★★★
These guys are good and professional!! Emma and George were easy to reach and readily responded to any questions throughout the credentialing process!
Date Jul 21, 2025
Meghan Immel
Public Counseling Services ✅
★★★★★
This group demonstrates excellent communication, punctual responses, attention to deadlines, and professionalism. They saved my business after Michigan medical billing compromised insurance payments.
Date Jul 21, 2025
Ghena Ribeiro
Present Moments ✅
★★★★★
Doctor Management Services has been awesome since I started working with them! They have been responsive and helpful with all my questions and worked super fast on getting me credentialed!
Date Jul 23, 2025
Maria Bennett
Psychiatric Nurse Practitioner ✅
★★★★★
Credentialing is usually one of the most stressful and time-consuming steps for new providers, so having someone like Alex at Doctor Management Services handle it smoothly is a huge relief.
Date Sep 10, 2025
Why Work With Doctor Management Services?
Medical credentialing shouldn’t slow down your practice.
By partnering with Doctor Management Services, you can:
- Save 100+ hours of paperwork & follow-ups
- Avoid missed deadlines and coverage lapses
- Reduce claim rejections and payment delays
- Focus more on patients—not paperwork
Get Expert Help — Risk-Free Consultation
Doctor MGT — Simplifying Credentialing. Ensuring Compliance. Helping Providers Get Paid Faster.
FAQs:
How do you manage CAQH and PECOS registration for new providers?
We create or update each provider’s CAQH and PECOS profiles, link their NPI and license details, and sync that information with payers to avoid enrollment delays. This ensures all data in both portals stays accurate and aligned with payer credentialing requirements.
What’s included in your NCQA compliance support?
Our credentialing company for physicians follows NCQA-approved verification procedures from primary-source checks to recredentialing reminders to keep your practice compliant with payer and accreditation standards. We also prepare you for NCQA or internal audits by maintaining documentation trails in real time.
How do you prevent data mismatches across credentialing systems?
Our team of doctor credentialing services makes sure to run automated cross-checks between CAQH, PECOS, and NPPES records to catch address, license, or taxonomy mismatches in credentialing services for providers before submission. This reduces payer rejections and keeps your medical credentialing records fully synchronized.
Can you handle credentialing updates for multi-state physicians or group practices?
Yes. Our medical credentialing services for providers cover single-state, multi-state, and multi-location setups. We track every board renewal, DEA registration, and state license update so your file stays active across all jurisdictions.
How often should my credentialing data be reviewed or revalidated?
We, as a medical credentialing company, recommend reviewing provider data every 90 days and performing full recredentialing every 2–3 years, depending on payer policy. Our platform automates these reminders, ensuring your physician credentialing stays current without interruptions.
What happens if a payer rejects an enrollment due to incomplete information?
Our team immediately audits the rejected application, fixes data errors, and resubmits it with the correct supporting documents. This minimizes lost time and ensures faster approval within insurance medical credentialing services workflows.
Do you assist with CAQH attestation and re-attestation reminders?
Absolutely. We monitor each provider’s attestation due date and handle re-attestation on schedule, keeping your CAQH file visible to payers at all times.
How do you ensure HIPAA compliance when managing credentialing data?
All documents are stored in encrypted, access-controlled systems with activity logs. Our credentialing company for physicians follows HIPAA’s Privacy and Security Rules, ensuring full protection of provider and patient-related data.
Can you integrate credentialing with my existing billing workflow?
Yes. Our medical billing and healthcare credentialing services are fully integrated credentialing data flows directly into payer enrollment and claim setup, preventing claim denials due to provider enrollment issues.
Are your credentialing operations based in California?
Yes. As one of the healthcare credentialing companies in California specializing in multi-specialty providers, we handle state-specific licensing, WC enrollments, and payer network setup for both individual doctors and group practices.

Talk to a growth expert