Healthcare professionals need to know how to recognize obstructive sleep apnea and its clinical consequences. The disease is categorized as G47.33 under ICD-10. This condition is challenging to diagnose and treat.
This blog gives a full explanation of obstructive sleep apnea (OSA). We will discuss the symptoms, diagnosis process, and other important aspects. The use of a uniform coding system helps practitioners manage and monitor various comorbidities, such as polypharmacy ICD-10. It is also an effective method for billing procedures.
After reading the blog, you will understand the clinical and healthcare aspects of OSA. You will then be able to explain the impact of ICD-10 G47.33 on medical documentation.
Overview of Obstructive Sleep Apnea
Obstructive sleep apnea is a sleep condition where the upper airway is either partially or wholly blocked during sleep. Such blockages can disrupt a person’s normal breathing pattern and make people wake up several times during the night.
OSA is the most common form of apnea and has its effects on people of all age groups, leading to various health issues. Low oxygen levels in the blood interrupt sleep. This triggers stress responses that can increase the risk of cardiovascular disease.
One of the most obvious symptoms of the disease is excessive daytime sleepiness. Other symptoms include loud snoring, morning headaches, dry mouth, and impairments in cognitive functions like the inability to concentrate.
Although OSA primarily affects adults, it can also affect children. Children with enlarged tonsils or obesity are more likely to develop this condition.
Prevalence of Obstructive Sleep Apnea
Obstructive sleep apnea (OSA) is a common sleep disorder. The prevalence of OSA in men is between 15% and 30%, while in women, it is between 10% and 15%. Uncontrolled weight gain is often linked to OSA.
Hence, treatments to shed off extra weight are essential. Symptoms of OSA often go unnoticed, especially when some of its side effects, like high blood pressure, Type 2 diabetes, and unnecessary medications, arise.
The negative effects of OSA on the health of patients are not limited to physical health only. Untreated OSA can lead to injuries at work, lower productivity, and social isolation due to tiredness. Early diagnosis and proper early medical management are therefore vital.
Understanding ICD-10 G47.33 and Its Importance
The International Classification of Diseases, Tenth Revision (ICD-10), places obstructive sleep apnea within the code number G47.33. This coding system allows healthcare professionals and billing teams to record diagnoses accurately. It also facilitates clear documentation of diagnoses. Correct usage ensures appropriate reimbursement. It also helps to reduce claim denials and keep patient records aligned with diagnostic standards.
Why ICD-10 G47.33 Is Relevant
The ICD-10 G47.33 code provides precise documentation of obstructive sleep apnea. This precision ensures uniform communication among all stakeholders. For instance, a respiratory therapist can use this classification in cooperation with sleep experts to provide customized treatments.
Hospitals can also track the OSA incidence among different cohorts of the population. Hence, they can implement tailored interventions for them.
Applications in Medical Billing
Proper coding eventually equates to efficient billing. Using the right ICD-10 codes in their medical billing claims, doctors ensure that their claims are in line with the requirements of the “payer.” This ensures the avoidance of administrative errors and promotes smooth insurance reimbursements.
Besides other functions, ICD-10 codes play a major role in med-legal issues. Sleep apnea is an important cause of work-related fatigue and traffic accidents. Claims of this sort usually carry the most weight when medics document the condition extensively, like OSA. This highlights the importance of comprehensive medical records.
How OSA is Diagnosed
Diagnosing obstructive sleep apnea needs teamwork. People often feel very sleepy during the day or say they don’t sleep well at night. Yet, these signs must be looked at closely before saying there is OSA.
The best way to know if someone has OSA is by doing a sleep study called polysomnography. This test measures brainwaves, oxygen levels, heartbeats, how you breathe, and muscle activity while asleep. Split-night sleep studies can be most helpful. In the first phase, they see how badly you breathe at night. If necessary, they use CPAP therapy in the second half of the test.
Some people prefer home sleep apnea testing (HSAT) because it is easier. But HSAT misses important details that lab studies find, so its accuracy varies a bunch based on the situation.
Furthermore, it’s crucial to recognize other conditions one may have. If someone has mental health problems, it makes diagnosis tougher. Psychiatrists need to check medical history cautiously for this reason too.
Treatment Approaches for Obstructive Sleep Apnea
Treating OSA focuses on addressing the airway obstructions and mitigating secondary health impacts. Treatment options typically fall into three categories—lifestyle changes, physical interventions, and surgical procedures.
Lifestyle Changes
For patients with mild OSA, lifestyle modifications can yield significant improvements. Weight loss through structured diet plans and exercise routines often reduces airway blockages. Avoiding alcohol and sedatives, especially before bedtime, also minimizes sleep disruptions.
Positive Airway Pressure Devices
CPAP machines are the most commonly used treatment for moderate to severe OSA. They create a constant flow of air that opens up the airway and allows the person to breathe freely during sleep. However, adhering to the treatment can be challenging for some patients. Informing patients about setting up the machine correctly and how to get rid of discomfort increases the rate of compliance.
Oral Appliances
For patients with mild OSA or those who find the mask uncomfortable to use, oral appliances can be a good alternative. Oral appliances try to relocate the tongue and lower jaw so that the passage of air is left undisturbed.
Surgical Options
For those who are struggling with moderate to severe sleep apnea, surgical options such as uvulopalatopharyngoplasty (UPPP) or maxillomandibular advancement (MMA) are sometimes required. Such treatments address the problem directly by modifying the airway, thus ensuring the person breathes effortlessly as he sleeps.
Key ICD-10 Codes Related to Sleep Apnea
While G47.33 is designated for obstructive sleep apnea, there are other ICD-10 codes covering different types of sleep apnea. This helps provide a differential diagnosis and documentation of the specific forms.
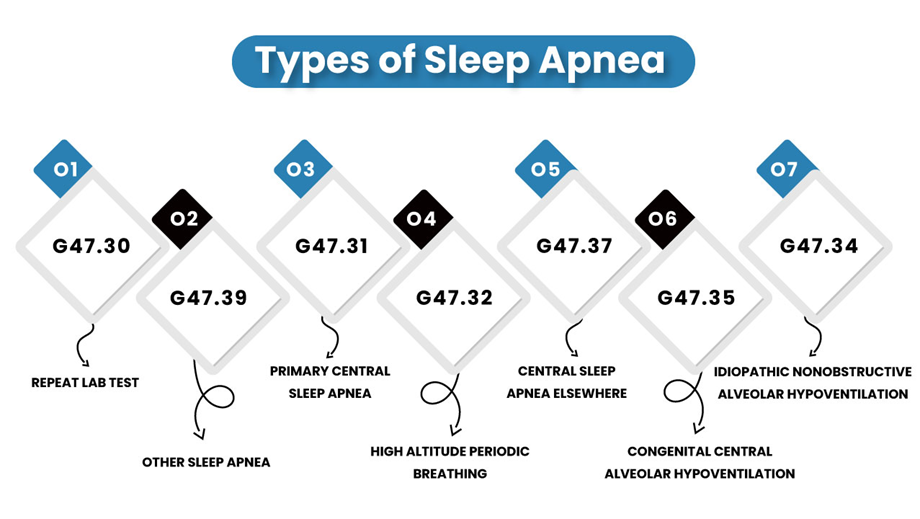
- G47.30 – Unspecified Sleep Apnea. This code applies when the type of sleep apnea is unclear. It may assist in preliminary diagnoses before further tests confirm specific categories.
- G47.31 – Primary Central Sleep Apnea. Unlike OSA, this condition occurs due to a lack of signals from the brain to the muscles that control breathing, rather than a physical obstruction.
- G47.32 – High Altitude Periodic Breathing. This form of sleep apnea is often seen in individuals acclimating to high altitudes, where oxygen levels are lower.
- G47.34 – Idiopathic Nonobstructive Alveolar Hypoventilation. This involves reduced oxygen intake and insufficient breathing without any identifiable obstruction.
- G47.35 – Congenital Central Alveolar Hypoventilation. A rare genetic condition affecting breathing during sleep.
- G47.37– G47.37: Central Sleep Apnea Elsewhere. Central sleep apnea associated with other medical conditions.
- G47.39– Other Sleep Apnea. Helpful in capturing less common variations. Sleep apnea not classified under any specific type or cause.
Uniting Clinical Insights with Improved Documentation
No matter if addressing polypharmacy cases, psychiatrist medical billing needs, or medical documentation, ICD-10 G47.33 is the link between clinical understanding and administrative efficiency. Healthcare professionals will only be able to achieve effective management by accurately coding the information and collaborative care strategies.