Smooth and efficient billing processes are the backbone of any successful medical practice. Healthcare providers and their billing staff alike should understand state-specific medical billing time limits. These deadlines, when you have to submit your claim, can vary widely by state, type of insurance, and the nature of the claim. Failing to meet or pay attention to these timelines may lead to the rejection of claims, the loss of money, and the redoing of work.
This guide breaks down what you need to know about clean claim in medical billing. Finding the definitions, key elements of clean claim, and specifying reasons for denials will help you master compliance, avoid expensive errors, and mitigate denials of claims.
What Is a Clean Claim in Medical Billing?
A clean claim is a submission made to an insurance company or payer that is free of error and has all the required information for processing. Clean claims are processed timely and do not face delays, rejections, or resubmissions.
Clean claims are essential for the healthcare revenue cycle to operate as planned, as they ensure that all necessary information is accurate and complete. Surgical claims, for example, bring additional intricacies associated with the correct coding mandated by ICD-10. When filed accurately, such claims lead to improved reimbursement and lower administrative costs.
In addition to its importance in maximizing reimbursement, clean claims also foster a relationship with payers due to professionalism and accuracy, setting the stage for claims to be processed much more easily in the future.
The Importance of Clean Claims in Healthcare Revenue Cycle Management
Regardless of their size or region, all healthcare organizations need a consistent revenue stream to stay financially viable. This revenue stream is driven by the submission of clean claims. Claim denials or rejections can lead to significant cash flow disruptions, damage the trust of providers, and add to administrative overhead.
Research has shown in Healthcare Finance News that more than 9% of medical claims are denied initially, costing providers an estimated $262 billion per year. Stronger processes and systems could prevent most of these denied claims. Clean claims increase the likelihood of avoiding these expensive denials, as well as saving time spent on resubmissions and appeals.
Aside from financial considerations, operational efficiency is greatly enhanced if claims are settled correctly in the first instance. Healthcare providers that adopt customized solutions, such as cardiology billing solutions, tend to get much more efficient and faster reimbursements from clean, streamlined submissions. Ultimately, these results lead to satisfaction and trust for your services.
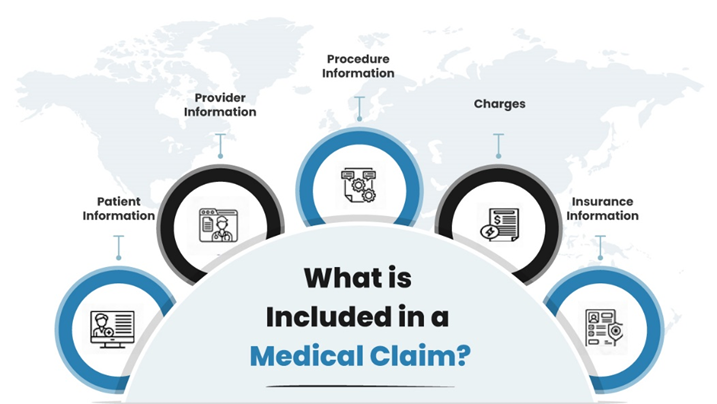
Key Elements of a Clean Claim
Accuracy and completion form the basis of a clean claim. Elements required for proper clean claims:
Accurate Patient Details: It is important that all the relevant information of a patient, including name, date and time of birth, contact number, insurance details, etc., is accurate. These variables may cause claims to be rejected if they do not match.
Correct Procedure and Diagnosis Codes: Use the correct codes, particularly ones that comply with the latest guidelines, such as ICD-10. Surgical Clearance ICD-10 is an example of specialty claims requiring an extra eye to ensure they are coded correctly.
Complete Supporting Documentation: If you work in a specialty practice, you must submit all medical reports, test results, and supporting documents for procedures performed.
Timely Submission: Timely submission must be followed by every provider, as delays in submission may cause automatic rejections.
Reasons for Claim Denials
Rejections don’t merely cause cash flow problems; they also tax administrative resources to argue for approvals. The first step toward avoiding these pitfalls is understanding the common reasons for them.
- Inaccurate patient information is one of the simplest mistakes to fix, but it persists in healthcare business office billing. Fatigue, the absence of strong checks, or just simple misunderstandings create small mistakes with major consequences.
- Medical coding gets updated every year. Obsolete or outdated codes applied to specialized claims for PI lien collections can contribute to the inaccurate reporting that produces denials.
- Submitting claims again without correcting errors from the initial submission can mark the claim as a duplicate.
- Lastly, a leading cause of denials continues to be a lack of proper medical records. This includes incomplete patient histories and missing laboratory results. This type of missing information is not only common, but it also significantly contributes to the payer’s inability to approve claims on time.
| Common Errors | Impact on Claim |
| Missing Patient Information | Rejection or Delay |
| Incorrect ICD-10 Codes | Denial for Incorrect Billing |
| Duplicate Claims Submission | Claim Flagging/Denial |
| Lack of Documentation | Denial for Insufficient Info |
Guide to Submitting a Clean Claim
A sound process is the first step to cleaner claim efficiency. Begin by effectively verifying patient data during the onboarding process. Making accurate entries minimizes mistakes later on in the revenue cycle.
Then, apply precise current ICD-10 coding to every identified condition and procedure. It’s crucial to educate yourself on coding changes for various claims, such as surgical clearance, to prevent any errors.
Next and certainly, comprehensive and organized documentation is equally important. In areas such as cardiology billing solutions, the final claim must include every single test result, x-ray, and physician’s note. Ensuring that these details align with the provided treatment can significantly reduce discrepancies in the future.
Finally, perform pre-submission audits with modern billing software. The tools available today use AI to detect potential errors and recommend fixes prior to submission. This proactive approach addresses most of the avoidable errors early on.
Specialized Billing Solutions for Niche Markets
Each specialty is unique, and the nuances of medical billing are no different—making specialty-specific solutions critical. Therefore, specialized solutions can improve clean claims rates in specific niche markets such as this one:
Cardiology: Claims related to diagnostic imaging, procedures, and interpretation require meticulous attention to detail. Besides, billing tools have advanced analytics in place to assign accurate procedure codes and avoid rejections.
Surgical Procedures: Claims based upon preoperative assessment ICD-10 codes are subject to unique challenges arising from strict procedural and documentation standards. Field-specific solutions simplify the process by ensuring compliance with coding standards.
PI Lien Claims: Personal injury lien claims can be intimidating without the appropriate tools. More technical platforms for lien collections help conform billing practices to legal standards and prevent documentation bottlenecks.
Tips for Boosting Clean Claim Rates
Education and training are investments that start the pathway to clean claims. Well-informed staff are the backbone of coding, documentation, and claim submission, ensuring to create a holistic approach to billing.
Moreover, frequent audits have a major effect, too. Because recurring errors are identified, those involved in care have the chance to implement changes that are more sustainable over time rather than a short-term fix.
In fact, implementing AI billing software is another game changer. These platforms minimize manual errors and enable scalability, which is a significant advantage. For specialties, utilizing expert billing companies that specialize in clean claim services ensures that practices maintain the confidence to face difficult claims head-on.
Achieving Operational Excellence Through Clean Claims
Clean claims are not only a technical requirement; they are the bedrock of operational excellence and a healthy practice. Seamless claims processing maintains a smooth revenue cycle and contributes to a positive patient experience. Imagine fewer billing disputes, less frustration regarding denied claims, and more delighted patients concentrating only on their recovery.
Being a healthcare provider, you can work to improve your clean claim rates by implementing comprehensive billing systems, complying with the latest ICD-10 coding standards, and utilizing tailor-fit solutions, such as billing solutions. For a low-risk (to you) means of improving the efficacy of your claim submissions, consider a professional billing service or an automation platform with proven efficacy—particularly in niche specialties (e.g., Personal injury lien collections, surgical billing).
Hence, a clean claim-first mindset can help healthcare providers optimize cash flow, reduce administrative overhead, and deliver the quality-of-care patients deserve. Examine your current billing systems today, considering how technology can revolutionize your entire process from beginning to end. Your practice’s efficiency—and your patients’ satisfaction—is at stake.