

With more than 20 years of experience in workers’ compensation, we don’t just handle bills, but we do it all, including RFAs, authorizations, billing, appeals, liens, Litigation, and payments. With the Doctor Management Services report, workers compensation collections made easier, we recover your lost revenue and bring it back directly to your pocket.
Tired of billing delays, denials, and past lien statutes? We handle worker’s compensation billing and collections, negotiations, Litigation, and settlements for you; every step, every claim, every code.
RCM Services
The Metrics Behind California’s Most Reliable WC Billing Team:
We Simplify Workers Compensation California, So You Get Paid Faster, Without the Stress.
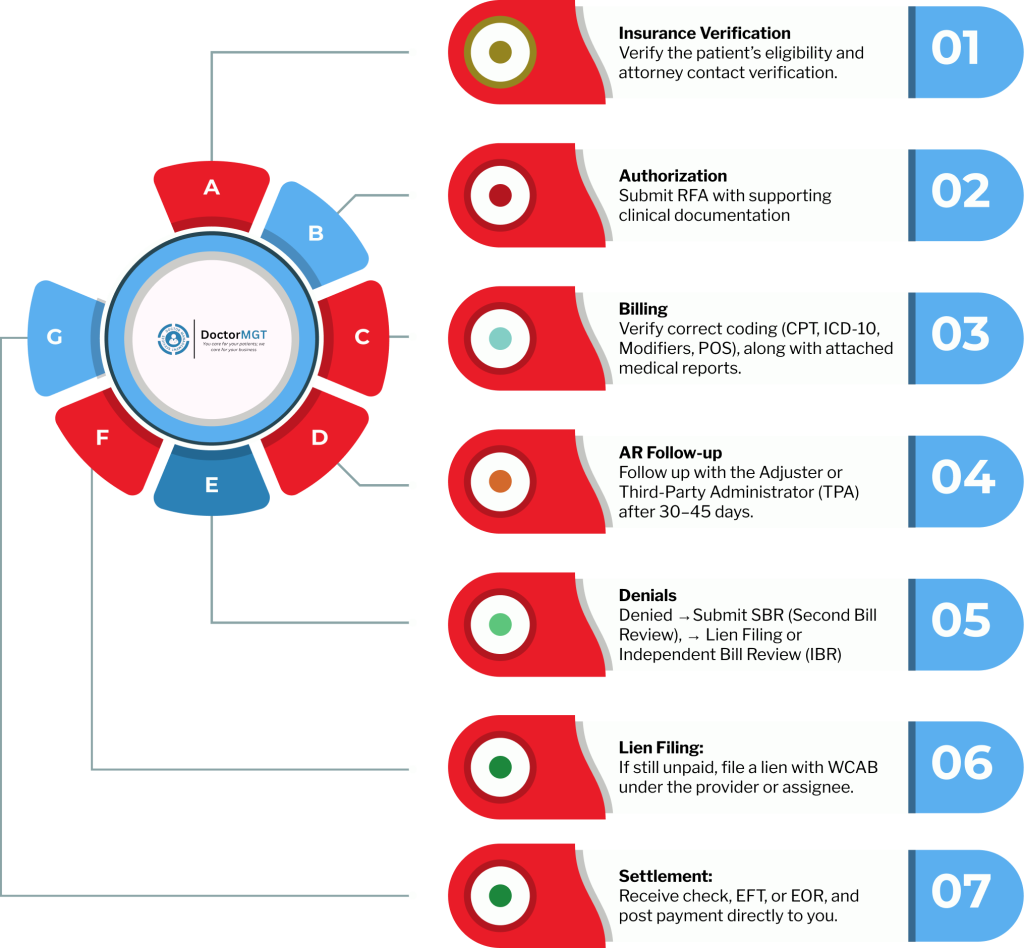
We handle every step of the Workers Comp process verification and authorization, billing and documentation, claims management, lien and settlement support.
Our workers compensation billing specialists verify every CPT, ICD, HCPCS, and modifier, and ensure HIPAA compliance.
We actively contact adjusters and carriers to get your claims paid faster, because we understand the importance of regular follow-up.
You’ll always know what’s paid, pending, or appealed; complete clarity on your collections and performance.
If you have any unpaid and aged claim that seems impossible to get paid, then don’t worry. Be Even. At Doctor Management Services, we take it further. As workers compensation billing experts, our Legal & Lien Enforcement team files, tracks, and negotiates your unpaid claims following the rules of California WCAB until you’re fully compensated. Now you focus on patients, we handle every step of the legal side.
Workers’ Compensation Litigation and legal proceedings can become quite hectic when not handled properly. Our Litigation & Legal Compliance Support services ensure your workers’ compensation matters are handled properly with regulatory adherence.
From managing lien disputes and preparing case documentation to representing your interests before the WCAB and ensuring full compliance with state-mandated requirements, we protect your revenue while minimizing the legal risks.
Our team of workers’ comp litigation professionals stays current with evolving Workers’ Compensation regulations, filing protocols, and procedural deadlines so your cases move forward efficiently and without costly delays.
Handling disputes when it comes to the Workers’ Compensation Appeals Board (WCAB) can be quite challenging. We fight your lien on your behalf. For this, Doctor management services provide hearing representation services throughout the USA. Our skilled representatives are available at every Workers’ Compensation Appeals Board (WCAB) to present your workers’ compensation claims effectively.
We offer services for hearing representation all around the USA. To guarantee that your interests are adequately represented, our knowledgeable representatives are on hand at any local Workers’ Compensation Appeals Board (WCAB).

In California workers’ comp, filing a lien isn’t just paperwork; it’s a legal step that must meet strict Division of Workers’ Compensation rules and be processed correctly in the Workers’ Compensation Appeals Board system. Even small mistakes can cause delays or dismissals. Workers’ Comp JET Filing Solutions helps providers with fast, compliant electronic filings, structured prep, validation checks, and real-time case tracking. We protect deadlines, reduce rejection risks, and keep cases moving. We don’t just submit liens; we handle them strategically to support your position.
Our Second Bill Review (SBR) and Reconsideration team thoroughly read each Explanation of Review (EOR) in detail to identify what went wrong and how to fix it.
We resubmit within California’s strict 60-day window, armed with documentation, fee-schedule references, and labor-code justification. If the carrier still doesn’t pay, we proceed to Lien Filing or Independent Bill Review (IBR) to protect your right to full compensation. As a workers’ compensation collection agency, every appeal is tracked, documented, and followed through until resolved.
Partner with the trusted workers’ compensation collection agency that actually brings real case insights and take help of local Workers’ Compensation expertise to help you recover faster.
Take control of your unpaid claims today with a workers’ compensation billing company that understands local Workers’ Compensation inside and out and turns complex cases into measurable results.
Let our experienced workers’ comp collections experts put strategies to work for you and start maximizing your recoveries now.
Doctor MGT utilizes a secure and efficient workers’ compensation collections system to track and manage stuck payments. We have premium workers’ compensation billing solutions that enable us to check your claims for any errors or discrepancies before submitting them to ensure minimal rejections and increased first-pass acceptance.
We handle the processing of all workers’ compensation claims seamlessly, whether it’s electronic or paper claims; providers trust us. As a workers’ compensation billing company, our relations with multiple clearinghouses enable us to submit claims electronically, ensuring efficient and accurate processing.
Workers’ Compensation Litigation and legal proceedings can become quite hectic when not handled properly. Our Litigation & Legal Compliance Support services ensure your workers’ compensation matters are handled properly with regulatory adherence.
From managing lien disputes and preparing case documentation to representing your interests before the WCAB and ensuring full compliance with state-mandated requirements, we protect your revenue while minimizing the legal risks.
Our team of workers’ comp litigation professionals stays current with evolving Workers’ Compensation regulations, filing protocols, and procedural deadlines so your cases move forward efficiently and without costly delays.
We follow a structured A/R workflow to keep your workers’ compensation claims moving. Initial follow-ups begin within 15–30 days of submission, aligned with payer response timelines. We review EOBs for underpayments based on fee schedules, correct coding or authorization issues, and resubmit documentation when needed.
Claims aging beyond 60–90 days are escalated for deeper review, including reconciliation, interest calculation where applicable, and lien preparation if required.
Every action is documented with clear audit trails and deadline tracking to stay compliant with WCAB procedures. The result is lower Days in A/R, fewer unresolved claims, and a clear path from submission to recovery.
Workers’ compensation payments can be delayed, denied, or simply fall through the cracks, and that directly impacts your revenue. That’s where DoctorMGT steps in. As your one complete solution for Workers’ Comp Billing & Collection services, we aggressively manage the entire collections process, follow up on every outstanding claim, and pursue every dollar you’ve rightfully earned. Stop chasing payments and start seeing results.
Partner with us today and take control of your Workers’ Comp revenue with confidence.
In professional workers’ compensation billing and collections, staying current with insurance plan updates and treatment guidelines is quite essential to maintain compliance and secure strong first-pass acceptance rates. With over 10 years of experience, our team delivers professional workers’ compensation billing solutions that reduce denials and consistently maximize reimbursements.
We specialize in resolving unpaid workers’ compensation liens through focused WC lien litigation for doctors, handling everything from initial lien perfection and DOR filings to courtroom representation. Our experienced workers’ compensation litigation team manages the entire legal process. Operating strictly within DWC guidelines, we work to secure timely, maximized payments for licensed medical providers across California.
Our legal team knows all the ins and outs of WC-38 filings, statutory liens, and perfected claims that fall under California labor codes. DoctorMGT provides dependable WC lien services that you can rely on from start to finish. With streamlined Workers Compensation Lien Jet Filing, we make sure every submission is accurate and completely aligned with DWC requirements and WCAB procedures.
\We help you reduce the denial rate under 3% and achieve up to a 97% First-Time Pass Rate with Doctor Management Services.
With DMS, no denied claim stays unresolved because we believe every legitimate service deserves to be paid. As one of the leading workers compensation billing company, here’s how we ensure that you get paid fairly for each of your claim:

Our Stats
Our Client’s Testimonials






Yes, our Workers Compensation Billing service covers complete. We manage both forms accurately based on your practice type. Whether you’re billing as a physician, ASC, or diagnostic facility, our team ensures every CMS-1500 or UB-04 is coded, verified, and filed according to California Workers Comp billing standards. Each submission includes the correct CPT, ICD-10, and modifier usage so your claims are accepted the first time, not bounced back for corrections
Absolutely. Our wc collections services in ca handle RFA submissions, UR approvals, and documentation management for every claim. Before submission, our workers compensation billing and collections team cross-checks that each bill includes the corresponding medical report, authorization letter, and any supporting forms required by the carrier or TPA. Our workers compensation billing service ensures compliance, reduces denials, and gives you peace of mind that every claim is fully supported from day one.
Yes, transparency is built into our Workers Compensation Billing service. You’ll receive detailed tracking reports that show every claim’s real-time status: submitted, accepted, pending, or paid. We keep providers informed through periodic summaries and live updates, so you always know where your revenue stands without having to call multiple adjusters or check multiple portals.
Yes, we manage the entire Second Bill Review (SBR) process for you. As soon as an EOR shows partial payment or denial, our team prepares and files the SBR within California’s 60-day deadline. Our workers compensation collections California team include all necessary CPT references, fee-schedule documentation, and Labor Code justification to strengthen the appeal and recover what’s owed. You won’t need to lift a finger during the process.
Yes, we maintain active follow-ups with clearinghouses and payers. Our medical billing workers compensation team monitors acceptance and rejection reports from platforms like Jopari, Optum, and Medata , quickly correcting any errors or resubmitting rejected files. We don’t just send bills and wait; our workers compensation collections team continuously track them until acknowledgment is confirmed and payment begins processing.
Yes, once workers compensation claims move into the appeal or lien phase, our team directly contacts insurance adjusters, defense counsel, and lien units to negotiate payments and resolve disputes. California workers compensation billing team handle communication professionally on your behalf, ensuring your rights are protected, documentation is clear, and every conversation moves your case closer to full reimbursement.
Absolutely, and as one of the best workers compensation billing companies, that’s what makes Doctor Management Services different. Our California workers compensation billing process includes a document-verification step before claim submission. Our coordinators reach out directly to your office in case any report, RFA, or authorization is missing. Our workers comp billing specialists maintain clear communication with your front desk or case manager so every claim leaves complete, compliant, and ready for payment the first time. It’s how we keep your revenue flowing without endless back-and-forth.
Yes, our team monitors your denials and catches the reason in billing for workers compensation with a focus on accuracy and compliance. After that, we thoroughly review all CPT, ICD-10, and modifier usage before submission, double-check documentation, and ensure authorizations are in place. By catching potential issues ahead of time, our WC collections services in CA reduce the likelihood of denials and speed up reimbursements.
Yes, 8 out of 10 providers trust Doctor Management Services for their workers compensation claims. As a workers comp collection agency in USA, we assist medical and healthcare providers, clinics, and hospitals across the country. Our workers comp collections process ensures consistent follow-up, timely payment, and complete documentation, even if it’s initial claim submission, appeals, or lien management.
We are the only workers’ comp collection agencies that offer complete workers’ compensation solutions. Our workers’ comp collections team ensures every claim is submitted accurately and followed up until payment is received. Our WC collections services in CA guarantee faster reimbursements and reduced claim denials.