

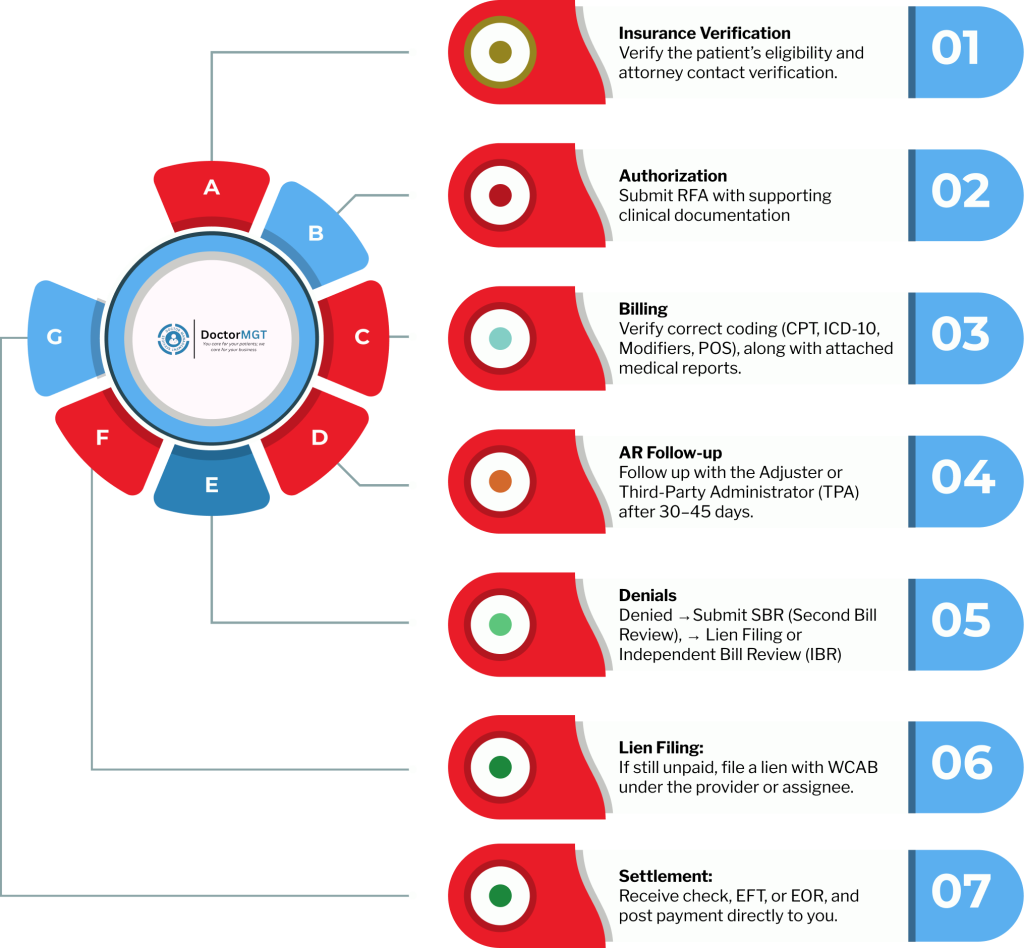
With more than 20 years of experience in workers’ compensation, we don’t just handle bills, but we do it all, including RFAs, authorizations, billing, appeals, liens, Litigation, and payments. With the Doctor Management Services report, workers compensation collections made easier, we recover your lost revenue and bring it back directly to your pocket.
Tired of billing delays, denials, and past lien statutes? We handle worker’s compensation billing and collections, negotiations, Litigation, and settlements for you; every step, every claim, every code.
RCM Services
The Metrics Behind California’s Most Reliable WC Billing Team:
We Simplify Workers Compensation California, So You Get Paid Faster, Without the Stress.
We handle every step of the Workers Comp process verification and authorization, billing and documentation, claims management, lien and settlement support.
Our workers compensation billing specialists verify every CPT, ICD, HCPCS, and modifier, and ensure HIPAA compliance.
We actively contact adjusters and carriers to get your claims paid faster, because we understand the importance of regular follow-up.
You’ll always know what’s paid, pending, or appealed; complete clarity on your collections and performance.
If you have any unpaid and aged claim that seems impossible to get paid, then don’t worry. Be Even. At Doctor Management Services, we take it further. As workers compensation billing experts, our Legal & Lien Enforcement team files, tracks, and negotiates your unpaid claims following the rules of California WCAB until you’re fully compensated. Now you focus on patients, we handle every step of the legal side.
Doctor Management Services has the experience and capabilities which are necessary to complete the claims settlement process quickly. We guarantee a 100% collection rate within 30 days of claim submission. Our workers comp collections experts have knowledge of AME (Agreed Medical Evaluation) and QME (Qualified Medical Evaluation) invoicing. Our team carefully reviews every bill to reduce the any possibility of rejection.

We designed an integrated workers’ compensation collections system to make your life easier and your practice more efficient. Our top-notch system of workers’ compensation claims collection takes all required information from EHR and uses it to pre-populate your workers comp claim forms. No more wasting time manually entering data or worrying about typo errors. It’s all done automatically, saving you precious time and ensuring accuracy.
Our professional litigation teams know the California workers’ compensation collection system inside out. They know how carriers think and use that insight to overturn denials, challenge reductions, and push claims through faster.
Our certified workers’ compensation billing specialists understand every CPT, ICD, and modifier rule from specialty-specific coding to California’s state-level nuances.
As a workers comp collection agency, we go beyond billing, escalating unresolved claims, filing liens, and negotiating settlements under California WC regulations to get you every dollar you’ve earned.
\We help you reduce the denial rate under 3% and achieve up to a 97% First-Time Pass Rate with Doctor Management Services.
With DMS, no denied claim stays unresolved because we believe every legitimate service deserves to be paid. As one of the leading workers compensation billing company, here’s how we ensure that you get paid fairly for each of your claim:

Our Stats
Our Client’s Testimonials






Yes, our Workers Compensation Billing service covers complete. We manage both forms accurately based on your practice type. Whether you’re billing as a physician, ASC, or diagnostic facility, our team ensures every CMS-1500 or UB-04 is coded, verified, and filed according to California Workers Comp billing standards. Each submission includes the correct CPT, ICD-10, and modifier usage so your claims are accepted the first time, not bounced back for corrections
Absolutely. Our wc collections services in ca handle RFA submissions, UR approvals, and documentation management for every claim. Before submission, our workers compensation billing and collections team cross-checks that each bill includes the corresponding medical report, authorization letter, and any supporting forms required by the carrier or TPA. Our workers compensation billing service ensures compliance, reduces denials, and gives you peace of mind that every claim is fully supported from day one.
Yes, transparency is built into our Workers Compensation Billing service. You’ll receive detailed tracking reports that show every claim’s real-time status: submitted, accepted, pending, or paid. We keep providers informed through periodic summaries and live updates, so you always know where your revenue stands without having to call multiple adjusters or check multiple portals.
Yes, we manage the entire Second Bill Review (SBR) process for you. As soon as an EOR shows partial payment or denial, our team prepares and files the SBR within California’s 60-day deadline. Our workers compensation collections California team include all necessary CPT references, fee-schedule documentation, and Labor Code justification to strengthen the appeal and recover what’s owed. You won’t need to lift a finger during the process.
Yes, we maintain active follow-ups with clearinghouses and payers. Our medical billing workers compensation team monitors acceptance and rejection reports from platforms like Jopari, Optum, and Medata , quickly correcting any errors or resubmitting rejected files. We don’t just send bills and wait; our workers compensation collections team continuously track them until acknowledgment is confirmed and payment begins processing.
Yes, once workers compensation claims move into the appeal or lien phase, our team directly contacts insurance adjusters, defense counsel, and lien units to negotiate payments and resolve disputes. California workers compensation billing team handle communication professionally on your behalf, ensuring your rights are protected, documentation is clear, and every conversation moves your case closer to full reimbursement.
Absolutely, and as one of the best workers compensation billing companies, that’s what makes Doctor Management Services different. Our California workers compensation billing process includes a document-verification step before claim submission. Our coordinators reach out directly to your office in case any report, RFA, or authorization is missing. Our workers comp billing specialists maintain clear communication with your front desk or case manager so every claim leaves complete, compliant, and ready for payment the first time. It’s how we keep your revenue flowing without endless back-and-forth.
Yes, our team monitors your denials and catches the reason in billing for workers compensation with a focus on accuracy and compliance. After that, we thoroughly review all CPT, ICD-10, and modifier usage before submission, double-check documentation, and ensure authorizations are in place. By catching potential issues ahead of time, our WC collections services in CA reduce the likelihood of denials and speed up reimbursements.
Yes, 8 out of 10 providers trust Doctor Management Services for their workers compensation claims. As a workers comp collection agency in USA, we assist medical and healthcare providers, clinics, and hospitals across the country. Our workers comp collections process ensures consistent follow-up, timely payment, and complete documentation, even if it’s initial claim submission, appeals, or lien management.
We are the only workers’ comp collection agencies that offer complete workers’ compensation solutions. Our workers’ comp collections team ensures every claim is submitted accurately and followed up until payment is received. Our WC collections services in CA guarantee faster reimbursements and reduced claim denials.