

It’s time to finally turn your medical bills into predictable revenue. Our certified billers help you do that by bringing 20+ years of expertise in coding, compliance, and claims, ensuring every detail, from correct ICD/ CPT/ HCPCS codes and modifiers to maintaining HIPAA standards. Everything is handled before the payer ever sees it; that’s how we maintain a 99% first-pass approval rate.
We review your billing structure, identify where revenue leaks begin, and fix them at the source. So you get consistent revenue and steady cash flow without chasing claims.
RCM Services
The metrics behind California’s most reliable medical billing agency:
Every healthcare provider faces unique billing challenges, and we handle them accordingly. Whether you are running a small clinic or managing hospitals, we provide medical billing services to every specialty.
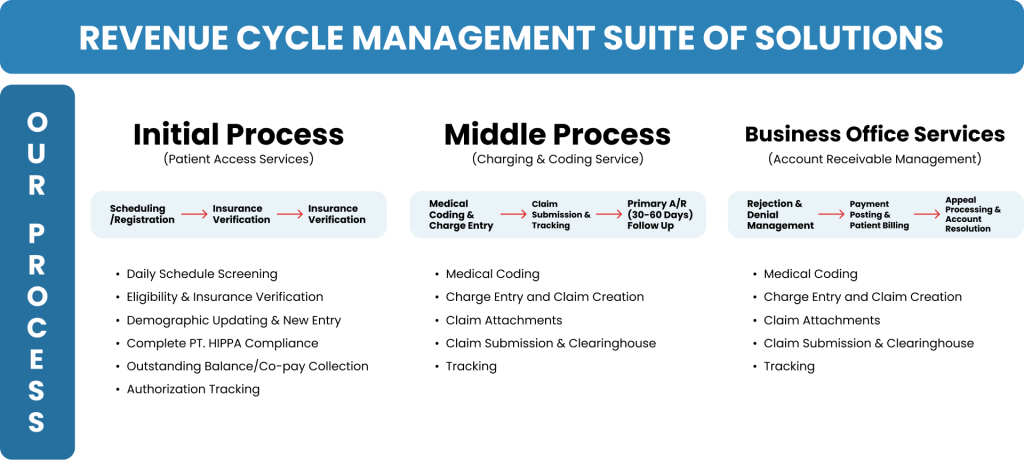
Our medical billing process starts with accurate documentation, passes through modifier alignment, and ends with payer-ready compliance, so you get fully reimbursed.
We validate every medical record, note, and attachment. Our Medical Billing and Coding Services California include it all, ready to submit.
As one of the leading medical billing companies in USA, our certified billers assign accurate CPT, ICD-10, and HCPCS codes.
Each claim passes a compliance audit for HIPAA compliance to ensure the privacy of the patient data and medical records.
After submission, we track every claim through payment. This includes regular follow-up and monitoring to ensure that your claims don’t get stuck.
We keep providers updated at every stage from claims submitted to payments posted, with transparent reports, real-time tracking, and complete visibility into your revenue cycle. With advanced billing systems and strict data security protocols, Doctor Management Services offers more than just billing. We are your dedicated partner for financial growth, ensuring every claim moves you closer to success.

Our billing process aligns with CMS and AMA coding standards while adapting to California’s unique payer and regulatory requirements.
Built on CMS and AMA coding frameworks. As the best medical billing company, our system is trusted, certified, and compliant.
With certified billers who ensure HIPAA compliance. Every claim is reviewed against the latest federal guidelines to maintain accuracy and audit readiness.
Clean, compliant submissions that meet payer expectations the first time. We stay aligned with California Workers’ Compensation and commercial payer rules to keep your claims moving without delays.
\We help you reduce the denial rate under 3% and achieve up to a 97% First-Time Pass Rate with Doctor Management Services.
Every stage of your billing process, from benefits verification to denial management, is managed by certified experts to ensure compliance, transparency, and full reimbursement. The Doctor Management Services redefines your medical billing experience through improving profitability, converting more A/R to cash, and working more efficiently.
We know accuracy matters; that’s why we start with accuracy at the very first step. By verifying each patient’s insurance coverage. Our team first checks each patient’s eligibility, deductibles, and authorization requirements before the appointments by calling or checking on the insurer’s website. After verifying benefits in advance, it reduces the chances of errors, avoids delays, and claim rejections.
Even a single digit entered incorrectly in the documentation can hold up a claim. Our California expert billing team carefully enters and validates patient demographics to ensure everything, from policy numbers to date of birth, is correct and consistent across your EHR and payer systems. This clean data upfront means smoother billing later.
What you get with Doctor Management Services:
Our AAPC-certified coders know the difference between similar procedures and how each one should be reported. That’s why we ensure proper and accurate ICD-10, CPT, and HCPCS coding along with their modifiers.
We code every document properly, including injection, ablation, and nerve block, in alignment with payer rules and medical documentation. That’s how we help you capture every dollar you’ve earned while staying fully compliant.
Missed charges? With Doctor MGT, every charge is posted on time.
Our billing specialists post charges directly from your operative and clinical reports, double-checking for completeness. Whether it’s an E/M visit, post-op follow-up, or multi-level procedure, nothing slips through our system.
Our professionals work in detail to ensure an accurate charge posting keeps your revenue predictable and your billing cycle smooth.
Speed and accuracy go hand in hand here at Doctor Management Services. We submit clean claims both electronically and one paper-based, usually within 24 hours of charge posting. Each claim is verified for coding errors and modifier accuracy before it ever reaches the payer. The result? Faster payments and far fewer denials to chase down later.
A/R follow-up is where many practices lose momentum and money. Our A/R team tracks every unpaid claim and follows up relentlessly until the balance is cleared. We review payer and insurance feedback thoroughly, identify recurring issues, and refile corrected claims quickly.
Because you should be paid for every service you provide.
We make sure that no payment slips through or go in vain. Firstly, we record insurance payments, patient co-pays, and adjustments in real time. We have a dedicated verification team that then verifies each entry against the Explanation of Benefits (EOB) to ensure accuracy. With us, you’ll always know what’s been paid and what’s pending.
We believe that you should know what is going on with your claims. That is why our customized reports give you clear insights into collection trends, denial patterns, and payer performance. Now, no confusing spreadsheets, just straightforward billing reports that help you see how your practice is performing and where you can optimize and increase financial growth.
You’ll know exactly how our billing process improves your bottom line, month after month, with our medical billing service California.
Our Stats
Our Client’s Testimonials






Accurate CPT, ICD-10, and HCPCS coding directly determines reimbursement success. Even a single incorrect code, modifier, or sequence can trigger automatic denials or underpayments. Our certified coders ensure every diagnosis and procedure code aligns with payer-specific requirements and California OMFS standards, maximizing claim acceptance on the first pass.
Most billing vendors only submit claims; we manage the entire revenue cycle. From documentation review and code validation to payer follow-up, denial resolution, and reporting, every stage is handled with precision. Our Medical billing services California include a process that integrates compliance checks, root-cause denial tracking, and detailed payer rule mapping, ensuring your billing is both compliant and profitable.
The best medical billing services combine precision, transparency, and advanced technology. When outsourcing, check whether they have a strong first-pass claim approval rate and proven expertise in your specialty.
Absolutely, as one of the best medical billing and coding companies in USA, we help you navigate claim denials. We perform denial pattern analysis to identify root coding errors, such as invalid code combinations, missing modifiers, or outdated CPT updates, and then correct, refile, and appeal claims with proper documentation. This approach routinely increases recovered payments by 20–40%.
Comprehensive medical billing and coding in the USA cover charge entry, coding compliance, claim submission, A/R follow-up, payment posting, and patient statement processing, all designed to improve efficiency and revenue.
Our medical billing management services workflow is built around CMS and AMA regulations. Every claim passes multiple validation layers from code-to-diagnosis accuracy to payer policy verification. We also run periodic audits to maintain full compliance with HIPAA, HITECH, and California Medical Board requirements.
Yes, we are a medical billing and coding company in California that manages complete administrative tasks for healthcare providers. Our medical billing service California, conducts detailed pre- and post-submission coding audits to detect discrepancies, outdated codes, and missing documentation. These audits improve compliance, reduce denials, and protect providers during payer or state-level reviews.
Yes, our system supports multi-specialty configurations from pain management, orthopedics, and neurology to surgery and diagnostic imaging. Each specialty is assigned dedicated coders trained in its specific billing nuances, ensuring accurate charge capture and faster reimbursements.
As one of the top medical billing companies in California, we track every claim from submission to final payment. Denied claims are analyzed for root cause, corrected immediately, and appealed within payer deadlines. Regular denial reports help identify recurring issues and improve future clean-claim rates.
Yes, our medical billing management services include regular audits and use claim-level analytics to detect missed codes, unbilled services, and underpayments. As a medical billing and coding company in California, we correct them at the source, improving cash flow and closing gaps that often go unnoticed in traditional billing setups.