

Does your credentialing get delayed without any reason? No worries anymore. Doctor Management Service helps physicians and healthcare providers get credentialed quickly and accurately. As a trusted medical credentialing company in Texas, we simplify the process and prevent costly enrollment delays so you can start seeing patients sooner. Our expert team delivers reliable physician credentialing services that Texas providers trust.
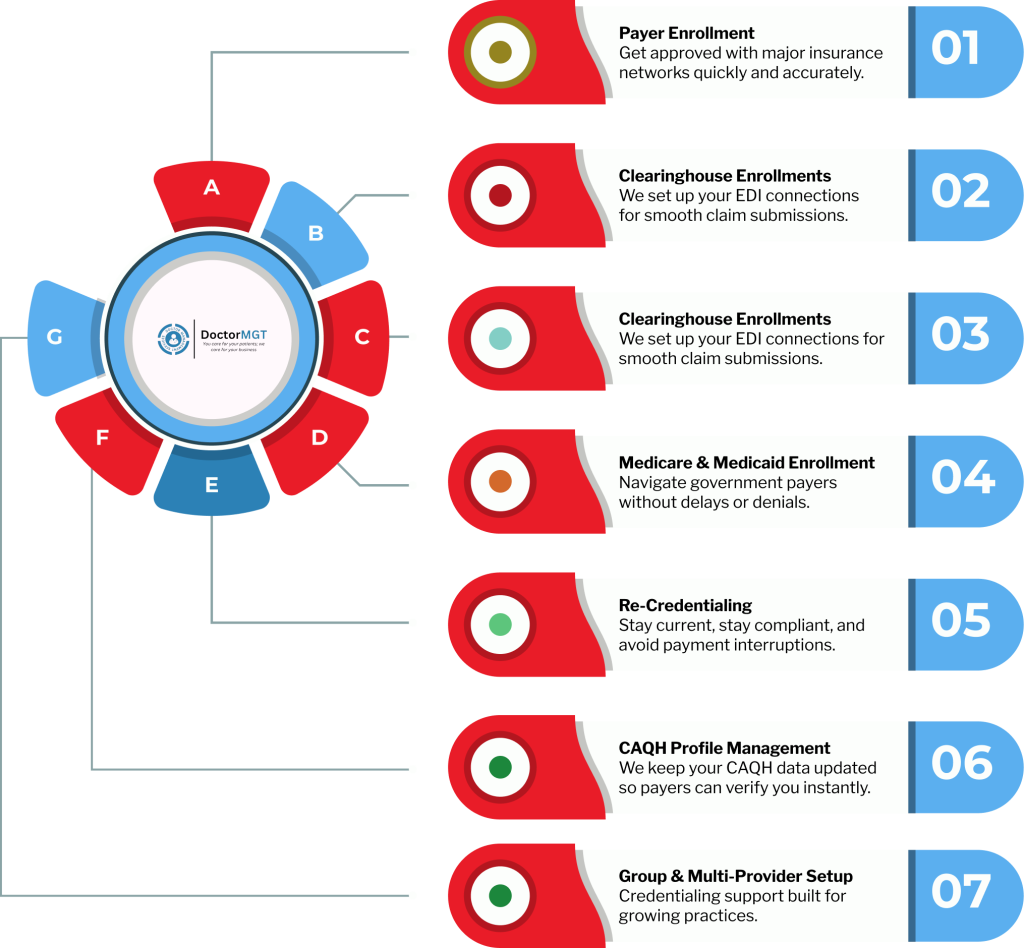
Credentialing Services
Whether you’re a solo provider or a hospital managing hundreds, we simplify the process for you.
Here is why more than 25000+ providers have trusted Doctor Management Services with medical credentialing services:
DoctorMGT delivers credentialing solutions that are designed for modern medical practices. Our approach is simple, transparent, and built to save your time so you can focus on delivering quality patient care.
Let us take hassle out of your healthcare credentialing, so you can concentrate on growing your practice
Enrolling your practice as a Medicare and Medicaid provider involves complex rules and regulations in Texas. DoctorMGT, as an experienced physician credentialing service in Texas, specializes in helping healthcare providers get Medicaid and Medicare credentials in 3x faster.
Having a correct and up-to-date NPI is vital for claims processing and electronic health records (EHR) exchange. We provide credentialing services assist healthcare providers for both Type 1 (individual) and Type 2 (organizational), in getting their National Provider Identifier (NPI).
Commercial insurance payers have different eligibility requirements and plans in Texas; the credentialing process might take a while. Experts at a physician credentialing company arrange all necessary paperwork, including licenses, certifications, and training records.
The complex paperwork, long approval timelines, frequent follow-ups with payers, missing documentation issues, and unexpected denials and delays patient onboarding and revenue. DoctorMGT is here to handle it all for you. We simplify the entire credentialing process.
Our Doctor credentialing services include reviewing every field, fixing outdated or missing data, and creating new CAQH ProView profiles when needed, ensuring your record is always accurate and enrollment-ready.
In the next step, we collect and upload all provider documents, licenses, and certifications while creating an enrollment file for data consolidation. All our files are password-protected and end-to-end encrypted to ensure compliance with the HIPAA data security rule.

We complete, validate, and submit applications to targeted insurance networks with zero data gaps, accelerating credentialing approvals and network activation.
Our physician credentialing team maintains constant communication with payers, resolves missing information requests immediately, and keeps providers in the USA updated until every application is approved.
We know credentialing can feel overwhelming, but we’re here to keep your credentials verified, compliant, and current, so you can focus on patients while we handle the details for you.
We oversee the creation and ongoing updates to the CAQH and PECOS credentialing portals.
We assure compliance with the NCQA standards through our provider credentialing services.
We maintain data integrity & contracting issues through regular audits.

Our Client’s Testimonials





Medical credentialing is the process of verifying a provider’s qualifications and enrolling them with insurance companies. Without credentialing, doctors cannot bill insurers, which can delay patient appointments and revenue.
Medical credentialing in Texas typically takes 60 to 120 days, depending on the payer, specialty, and completeness of documentation. Working with experienced medical credentialing services Texas providers trust can help reduce delays.
Insurance credentialing services include completing applications, verifying licenses and certifications, submitting documents to payers, and following up until approval. Some providers also offer ongoing maintenance and re-credentialing support.
You can do it yourself, but many providers choose a credentialing company for physicians to save time, avoid errors, and speed up approvals. Credentialing specialists understand payer requirements and handle complex follow-ups.
Yes, many practices prefer combined medical billing and credentialing services in Texas to streamline operations, reduce administrative burden, and improve cash flow.
Common documents include medical license, DEA registration, board certification, malpractice insurance, NPI number, CV, and identification. Requirements may vary by payer and specialty.
Most insurance companies require re-credentialing every 2–3 years. Ongoing support from a medical credentialing company in Texas helps ensure credentials stay active without interruptions.
Yes, credentialing services for providers often include nurse practitioners, physician assistants, behavioral health providers, and other healthcare professionals.
Common challenges include missing documents, payer delays, changing regulations, and communication gaps. Professional Texas healthcare credentialing support helps prevent these issues.
You can start by submitting your provider information and required documents. A credentialing specialist will prepare applications, submit them to payers, and manage the entire process for you.